COVID-19 and Cardiac Injury: A Complex Interplay
Keywords:
Coronavirus disease 2019, COVID-19, SARS-CoV-2, Cardiovascular disease, Cardiac injuryAbstract
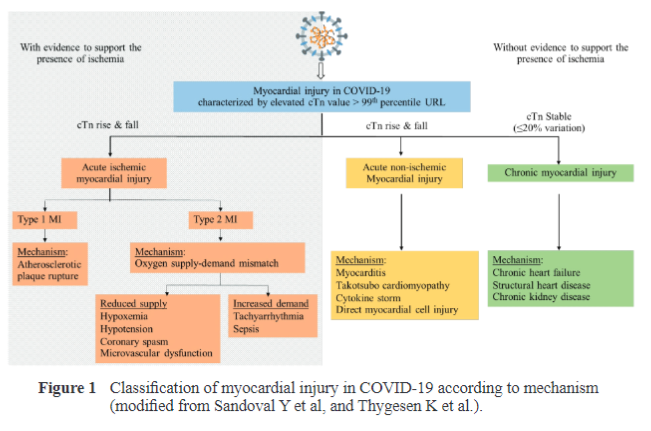
Although the coronavirus disease-2019 (COVID-19) primarily affects the respiratory system, the cardiovascular system is the potential target since angiotensin-converting enzyme 2 (ACE2), which acts as a receptor for the virus, is also extensively expressed in the myocardium. A large proportion of individuals infected with COVID-19 have prior cardiac risk factors in which hypertension and diabetes are the most prevalent comorbidities. Cardiac injury, defined as an elevated cardiac troponin, is the most reported cardiac abnormality in COVID-19. Acute cardiac injury can occur through a number of possible mechanisms include: (1) Non-ischemic myocardial injury related to various causes e.g., systemic inflammation, cytokine storm, stress-induced cardiomyopathy, and myocarditis. (2) Ischemic cardiac injury related to different pathophysiology e.g., plaque rupture, coronary spasm, or myocardial oxygen demand-supply mismatch. Cardiovascular disease and COVID-19 have a complex interplay. The presence of preexisting cardiovascular disease increasessusceptibility to COVID-19 infection as well as morbidity and mortality. On the other hand, COVID-19 infection can worsen the underlying cardiovascular disease or even trigger new complications, such as myocardial injury, which is closely related to the disease progression and prognosis.
Downloads
References
Wu Z, McGoogan JM. Characteristics of and Important Lessons from the Coronavirus Disease 2019 (COVID-19) Outbreak in China:
Summary of a Report of 72 314 Cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;323(13):1239-1242.
Teixeira R, Santos M, Gil V. COVID-19 and cardiovascular comorbidities: An update. Rev Port Cardiol (Engl Ed). 2020;39(8):417-419.
Cui J, Li F, Shi ZL. Origin and evolution of pathogenic coronaviruses. Nat Rev Microbiol. 2019;17(3):181-192.
Zaki AM, van Boheemen S, Bestebroer TM, Osterhaus AD, Fouchier RA. Isolation of a novel coronavirus from a man with pneumonia in Saudi Arabia. N Engl J Med. 2012;367(19):1814-1820.
Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497-506.
Tajbakhsh A, Gheibi Hayat SM, Taghizadeh H, et al. COVID-19 and cardiac injury: clinical manifestations, biomarkers, mechanisms, diagnosis, treatment, and follow up. Expert Rev Anti Infect Ther. 2021;19(3):345-357.
Gencer S, Lacy M, Atzler D, van der Vorst EPC, Doring Y, Weber C. Immunoinflammatory, Thrombohaemostatic, and Cardiovascular Mechanisms in COVID-19. Thromb Haemost. 2020;120(12):1629-1641.
Chung MK, Zidar DA, Bristow MR, et al. COVID-19 and Cardiovascular Disease: From Bench to Bedside. Circ Res. 2021;128(8):1214-1236.
Zheng YY, Ma YT, Zhang JY, Xie X. COVID-19 and the cardiovascular system. Nat Rev Cardiol. 2020;17(5):259-260.
Yang J, Zheng Y, Gou X, et al. Prevalence of comorbidities and its effects in patients infected with SARS-CoV-2: a systematic review and meta-analysis. Int J Infect Dis. 2020;94:91-95.
Li B, Yang J, Zhao F, et al. Prevalence and impact of cardiovascular metabolic diseases on COVID-19 in China. Clin Res Cardiol. 2020;109(5):531-538.
Kang Y, Chen T, Mui D, et al. Cardiovascular manifestations and treatment considerations in COVID-19. Heart. 2020;106(15):1132-1141.
Lang JP, Wang X, Moura FA, Siddiqi HK, Morrow DA, Bohula EA. A current review of COVID-19 for the cardiovascular specialist. Am Heart J. 2020;226:29-44.
Guzik TJ, Mohiddin SA, Dimarco A, et al. COVID-19 and the cardiovascular system: implications for risk assessment, diagnosis, and treatment options. Cardiovasc Res. 2020;116(10):1666-1687.
Gheblawi M, Wang K, Viveiros A, et al. Angiotensin-Converting Enzyme 2: SARS-CoV-2 Receptor and Regulator of the ReninAngiotensin System: Celebrating the 20th Anniversary of the Discovery of ACE2. Circ Res. 2020;126(10):1456-1474.
Rowland B, Kunadian V. Challenges in the management of older patients with acute coronary syndromes in the COVID-19 pandemic. Heart. 2020;106(17):1296-1301.
Ferrario CM, Jessup J, Chappell MC, et al. Effect of angiotensin-converting enzyme inhibition and angiotensin II receptor blockers on cardiac angiotensin-converting enzyme 2. Circulation. 2005;111(20):2605-2610.
Bavishi C, Maddox TM, Messerli FH. Coronavirus Disease 2019 (COVID-19) Infection and Renin Angiotensin System Blockers. JAMA
Cardiol. 2020;5(7):745-747.
Williams B, Mancia G, Spiering W, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. J Hypertens. 2018;36(10):1953-2041.
ESH. ESH statement on COVID-19. Eshonline. https://www.eshonline.org/spotlights/esh-statement-on-covid-19. Published March 12, 2020. Accessed October 10, 2021.
American College of Cardiology. HFSA/ACC/AHAStatementAddresses Concerns Re: Using RAAS Antagonists in COVID-19. American College of Cardiology. https://www.acc.org/latest-in-cardiology/articles/2020/03/17/08/59/hfsa-acc-aha-statement-addresses-concernsre-using-raas-antagonists-in-covid-19. Published March 17, 2020. Accessed October 10, 2021.
Position Statement of the ESC Council on Hypertension on ACE-Inhibitors and Angiotensin Receptor Blockers. https://www.escardio.org/Councils/Council-on-Hypertension-(CHT)/News/position-statementof-the-esc-council-on-hypertension-on-aceinhibitors-and-ang. Published March 13, 2020. Accessed October 10, 2021.
Hypertension Canada’s Statement on: Hypertension, ACE-Inhibitors and Angiotensin Receptor Blockers and COVID-19. https://hypertension.ca/wp-content/uploads/2020/03/2020-30-15-Hypertension-Canada-Statement-on-COVID-19-ACEiARB.pdf Published March 13, 2020.Accessed October 10, 2021.
COVID-19 and concerns regarding use of ACEi/ARB/ARNi medicationsfor heart failure or hypertension. https://www.ccs.ca/images/Images_2020/CCS_CHFS_state-mentregarding_COVID_EN.pdf. Published March 15, 2020. Accessed October 10, 2021.
A statement from the International Society of Hypertension on COVID-19. https://ish-world.com/news/a/A-statement-fromthe-International-Society-of-Hypertensionon-COVID-19. Published March 16, 2020. Accessed October 10, 2021.
BSH & BCS Joint statement on ACEi or ARB in relation to COVID-19. https://www.britishcardiovascularsociety.org/news/
ACEi-or-ARB-and-COVID-19 Published March 19, 2020. Accessed October 10, 2021.
Bansal M. Cardiovascular disease and COVID-19. Diabetes Metab Syndr. 2020;14 (3):247-250.
Shi S, Qin M, Shen B, et al. Association of Cardiac Injury With Mortality in Hospitalized Patients With COVID-19 in Wuhan, China.
JAMA Cardiol. 2020;5(7):802-810.
Thygesen K, Alpert JS, Jaffe AS, et al. Fourth Universal Definition of Myocardial Infarction (2018). Circulation. 2018;138(20):618-651.
Sahoo S,MehraA,Grover S. StressCardiomyopathy/Takotsubo Syndrome and COVID-19: An Important Link to Understand. Indian Journal of Clinical Cardiology. 2021;2(2):124-125.
Tavazzi G, Pellegrini C, Maurelli M, et al. Myocardial localization of coronavirus in COVID-19 cardiogenic shock. Eur J Heart Fail. 2020;22(5):911-915.
Van Linthout S, Klingel K, Tschope C. SARS-CoV-2-related myocarditis-like syndromes Shakespeare's question: what's in a name? Eur J Heart Fail. 2020;22(6):922-925.
Guo T, Fan Y, Chen M, et al. Cardiovascular Implications of Fatal Outcomes of Patients With Coronavirus Disease 2019 (COVID-19). JAMA Cardiol. 2020;5(7):811-818.
Madjid M, Safavi-Naeini P, Solomon SD, Vardeny O. Potential Effects of Coronaviruses on the Cardiovascular System: A Review. JAMA Cardiol. 2020;5(7):831-840.
Sandoval Y, Januzzi JL Jr, Jaffe AS. Cardiac Troponin for Assessment of Myocardial Injury in COVID-19: JACC Review Topic of the Week. J Am Coll Cardiol. 2020;76(10):1244-1258.
Kwong JC, Schwartz KL, Campitelli MA, et al. Acute Myocardial Infarction after Laboratory Confirmed Influenza Infection. N Engl J Med. 2018;378(4):345-353.
Matsushita K, Marchandot B, Jesel L, Ohlmann P, Morel O. Impact of COVID-19 on the Cardiovascular System:AReview. J Clin Med.
;9(5):1407.
Esfandiarei M, McManus BM. Molecular biology and pathogenesis of viral myocarditis. Annu Rev Pathol. 2008;3:127-155.
Siripanthong B, Nazarian S, Muser D, et al. Recognizing COVID-19-related myocarditis: The possible pathophysiology and proposed guideline for diagnosis and management. Heart Rhythm. 2020;17(9):1463-1471.
Ho JS, Sia CH, Chan MY, Lin W, Wong RC. Coronavirus-induced myocarditis: A meta-summary of cases. Heart Lung.
;49(6):681-685.
Salah HM, Mehta JL. Takotsubo cardiomyopathy and COVID-19 infection. Eur Heart J Cardiovasc Imaging. 2020;21(11):1299-1300.
Meyer P, Degrauwe S, Van Delden C, Ghadri JR, Templin C. Typical takotsubo syndrome triggered by SARS-CoV-2 infection. Eur Heart J. 2020;41(19):1860.
Sala S, Peretto G, Gramegna M, et al. Acute myocarditis presenting as a reverse Tako-Tsubo syndrome in a patient with SARS-CoV respiratory infection. Eur Heart J. 2020;41(19):1861-1862.
Sinha P, Matthay MA, Calfee CS. Is a “Cytokine Storm” Relevant to COVID-19? JAMA Intern Med. 2020;180(9):1152-1154.
Fajgenbaum DC, June CH. Cytokine Storm. N Engl J Med. 2020;383(23):2255-2273.
Del Valle DM, Kim-Schulze S, Huang HH, et al. An inflammatory cytokine signature predicts COVID-19 severity and survival. Nat
Med. 2020;26(10):1636-1643.
Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054-1062.
Bavishi C, Bonow RO, Trivedi V, Abbott JD, Messerli FH, Bhatt DL. SpecialArticle -Acute myocardial injury in patients hospitalized with COVID-19 infection: A review. Prog Cardiovasc Dis. 2020;63(5):682-689.
Aboughdir M, Kirwin T, Abdul Khader A, Wang B. Prognostic Value of Cardiovascular Biomarkers in COVID-19: AReview. Viruses. 2020;12(5):527.
Giustino G, Croft LB, Stefanini GG, et al. Characterization of Myocardial Injury in Patients with COVID-19. J Am Coll Cardiol. 2020;76(18):2043-2055.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2022 Asian Medical Journal and Alternative Medicine

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.


