Delayed Cord Clamping Effects, with or without Umbilical Cord Milking, on Premature Infant Hemodynamic Circulation: A Randomized Control Trial
Keywords:
Delayed cord clamping, Placental transfusion, Preterm infants, Systemic blood flow, Umbilical cord milkingAbstract
Introduction: Delayed cord clamping (DCC) results in decreased incidence of intraventricular hemorrhage (IVH) by increasing the systemic blood flow which is assessed by measuring superior vena cava (SVC) flow, right ventricular (RV) output and left ventricular (LV) output. Umbilical cord milking (UCM) is an alternative placental transfusion method with higher levels of systemic blood flow. We intend to explore if UCM can augment DCC benefits.
Objectives: To compare placental transfusion hemodynamic effects between 3 techniques: DCC, DCC with UCM before clamping (DCM-B), and DCC with UCM after cord clamping (DCM-A).
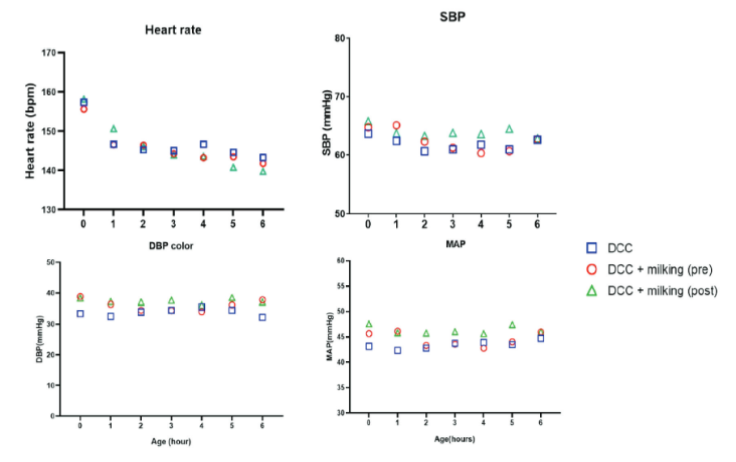
Methods: Premature infants at 28-33 weeks GA born at Thammasat University Hospital were randomized by placental transfusion methods. Vital signs were recorded, and blinded echocardiography was performed to evaluate hemodynamic circulation within 24 hours of age.
Results: One hundred and twenty infants were divided into 3 groups. No significant differences in incidence of intraventricular hemorrhage (IVH) were observed between groups and no severe IVH had occurred. DCC group had higher SVC flow (150.9 ± 81.1 mL/kg/min), RV output (271.3 ± 110.4 mL/kg/min), and LV output (232.4 ± 81.6 mL/kg/min) in comparison to DCM-B and DCM-A group but were not statistically significant.
Conclusions: Our study showed DCC with or without UCM had no significant variations in hemodynamic effects and may benefit preterm infants. DCC combined with UCM appeared to be safe with none of the participants developing severe IVH.
Downloads
References
Al-Wassia H, Shah PS. Efficacy and safety of umbilical cord milking at birth: a systematic review and meta-analysis. JAMA Pediatr. 2015;169:18-25.
Hosono S, Mugishima H, Fujita H, et al. Blood pressure and urine output during the first 120 h of life in infants born at less than 29 weeks’ gestation related to umbilical cord milking. Arch Dis Child Fetal Neonatal Ed. 2009;94:328-331.
Goldberg RN, Chung D, Goldman SL, Bancalari E. The associations of rapid volume expansion and intraventricular hemorrhage in the preterm infant. J Pediatr. 1980;96;1060-1063.
Hill A, Perlman JM, Volpe JJ. Relationship of pneumothorax to the occurrence of intraventricular hemorrhage in the premature newborn. Pediatrics. 1982;69:144-149.
Perlman JM, McMenamin JB, Volpe JJ. Fluctuating cerebral blood flow velocity in respiratory distress syndrome. Relation to the development of intraventricular hemorrhage. N Engl J Med. 1983;309:204-209.
Kluckow M, Evans N. Relationship between blood pressure and cardiac output in preterm infants requiring mechanical ventilation. J Pediatr. 1996;129:506-512.
Kluckow M, Evans N. Low superior vena cava flow and intraventricular haemorrhage in the preterm infant. Arch Dis Child Fetal Neonatal Ed. 2000;82:188-194.
Katheria AC, Truong G, Cousins L, Oshiro B, Finer NN. Umbilical cord milking versus delayed cord clamping in preterm infants. Pediatrics. 2015;136:61-69.
American College of Obstetricians and Gynecologists’ Committee on Obstetric Practice. Delayed Umbilical Cord Clamping After Birth: ACOG Committee Opinion, Number 814. Obstet Gynecol. 2020;136:100-106.
Kluckow M, Evans N. Superior vena cava flow in newborn infants: a novel marker of systemic blood flow. Arch Dis Child Fetal Neonatal Ed. 2000;82:182-187.
Meye MP, Midildenhall L. Delayed cord clamping and blood flow in the superior vena cava in preterm infants: an observational study. Arch Dis Child Fetal Neonatal Ed. 2012;97:484-486.
Alan S, Arsan S, Okulu E, et al. Effects of umbilical cord milking on the need for packed red cell transfusions and early neonatal hemodymamic adaptation in preterm infants born ≤1500 g: a prospective, randomized, controlled trial. J Pediatr Hematol Oncol. 2014;36:493-498.
Popat H, Robledo KP, Sebastian L, et al. Effect of delayed cord clamping on systemic blood flow: A randomized controlled trial. J Pediatr. 2016;178:81-86.
Hosono S, Mugishima H, Fujita H, et al. Umbilical cord milking reduces the need for red cell transfusions and improves neonatal adaptation in infants born at less than 29 weeks’gestation: a randomised controlled trial. Arch Dis Child Fetal Neonatal Ed. 2008;93:14-19.
Heuchan AM, Evans N, Henderson Smart DJ, Simpson JM. Perinatal risk factors for major intraventricular haemorrhage in the Australian and New Zealand Neonatal Network, 1995-1997. Arch Dis Child Fetal Neonatal Ed. 2002;86:86-90.
Jasani B, Torgalkar R, Ye XY, Syed S, Shah PS. Association of umbilical cord management strategies with outcomes of preterm Infants: A systematic review and network meta-analysis. JAMA Pediatr. 2021;175:e210102.
Katheria A, Reister F, Essers J, et al. Association of Umbilical Cord Milking vs Delayed Umbilical Cord Clamping with death or severe Intraventricular Hemorrhage Among Preterm Infants. JAMA. 2019;322:1877-1886.
Krueger MS, Eyal FG, Peevy KJ, Hamm CR, Whitehurst RM, Lewis DF. Delayed cord clamping with and without cord stripping: a prospective randomized trial of preterm neonates. Am J Obstet Gynecol. 2015;212(3):394.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2022 Asian Medical Journal and Alternative Medicine

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.


