Operation Time for Pterygium Surgery by Ophthalmology Trainees
Keywords:
Pterygium surgery, Ophthalmology resident, Operation time, Surgical skill, Skill developmentAbstract
Objective: To evaluate the duration time of pterygium surgery performed by the ophthalmology residents in the first and second year of training with different surgical methods.
Methods: Data was collected retrospectively from medical records when the surgeons were first-year residents in 2016 and second-year in 2017. Operation time was compared according to each resident surgeon, year level of training, and surgical techniques.
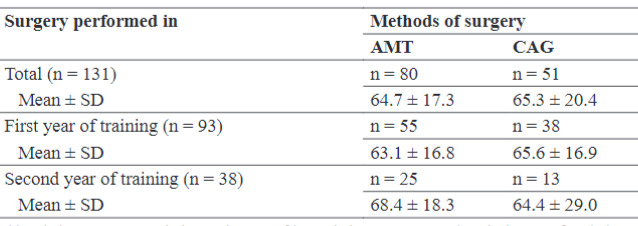
Results: A total of 131 pterygium surgeries were performed by 5 ophthalmology residents, 93 and 38 pterygium excision procedures were performed by one group of residents in their first and second year of training, respectively. All pterygia were primary type with a single head. The mean pterygium size was 2.8 ± 1.4 mm. The range of operating duration was 52 - 83 minutes for individual surgeons. The mean duration of surgery performed by the first- and second-year residents was 64.1 ± 16.8 and 67.0 ± 22.2 minutes, respectively. The mean duration of surgery operated with amniotic membrane and conjunctival graft techniques were 64.7 ± 7.3 and 65.3 ± 20.4 minutes, respectively. The duration times of pterygium surgery were significantly different (P < .001) between surgeons but there were no statistically significant differences with regards to the level of training and method of surgery
(P > .05).
Conclusions: The duration of pterygium surgery varied between each resident surgeon, but did not differ in the level of training and surgical techniques.
Downloads
References
Singh SK. Pterygium: epidemiology prevention and treatment. Community Eye Health. 2017;30(99):S5-S6.
Nangia V, Jonas JB, Nair D, Saini N, Nangia P, Panda-Jonas S. Prevalence and associated factors for pterygium in rural agrarian central India. The central India eye and medical study. PLoS One. 2013;8(12):e82439.
Malozhen SA, Trufanov SV, Krakhmaleva DA. Pterygium: etiology, pathogenesis, treatment. Vestn Oftalmol. 2017;133(5):76-83.
Wanzeler ACV, Barbosa IAF, Duarte B, et al. Mechanisms and biomarker candidates in pterygium development. Arq Bras Oftalmol. 2019;82(6):528-536.
Akrapipatkul K, Kupakanjana T, Charoenphol P.Efficiency in skill development of pterygium excision with amniotic membrane transplantation among the 1st year ophthalmology residents at Thammasat Eye Center. EyeSEA. 2019;14(2):70-81.
Kositphipat K, Tananuvat N, Choovuthayakorn J. Results of pterygium excision adjunct with conjunctival autograft transplantation for primary pterygium by ophthalmology trainees. Int Ophthalmol. 2016;36(5):615-621.
Phrueksaudomchai P, Patarajierapan P, Leelawongtawun W, et al. Surgical time aspect of learning curve in primary pterygium excision by ophthalmology trainees. EyeSEA. 2021;16(1):94-103.
Koranyi G, Artzén D, Wijk T. Learning curve in the Cut and Paste method for surgery of primary pterygium. Acta Ophthalmol.
;91(5):463-468.
Karalezli A, Kucukerdonmez C, Akova YA, Altan-Yaycioglu R, Borazan M. Fibrin glue versus sutures for conjunctival autografting in
pterygium surgery: a prospective comparative study. Br J Ophthalmol. 2008;92(9):1206-1210.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2022 Asian Medical Journal and Alternative Medicine

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.


