Telomere Length in Various Age Groups of Normal-Body Weight Thais and Obese Thais
Keywords:
Telomere length, Obesity, Body weight, Age groups, Nutritional statusAbstract
Introduction: Telomere is non-coding nucleoprotein at the terminal of chromosomes that shortens during DNA replication as a cause of aging. In obese people, excess body fat is a key role in inducing chronic inflammation which accelerates telomere shortening. This study aimed to determine the difference in telomere length between normal body weight and obese Thais males aged 21-82 years.
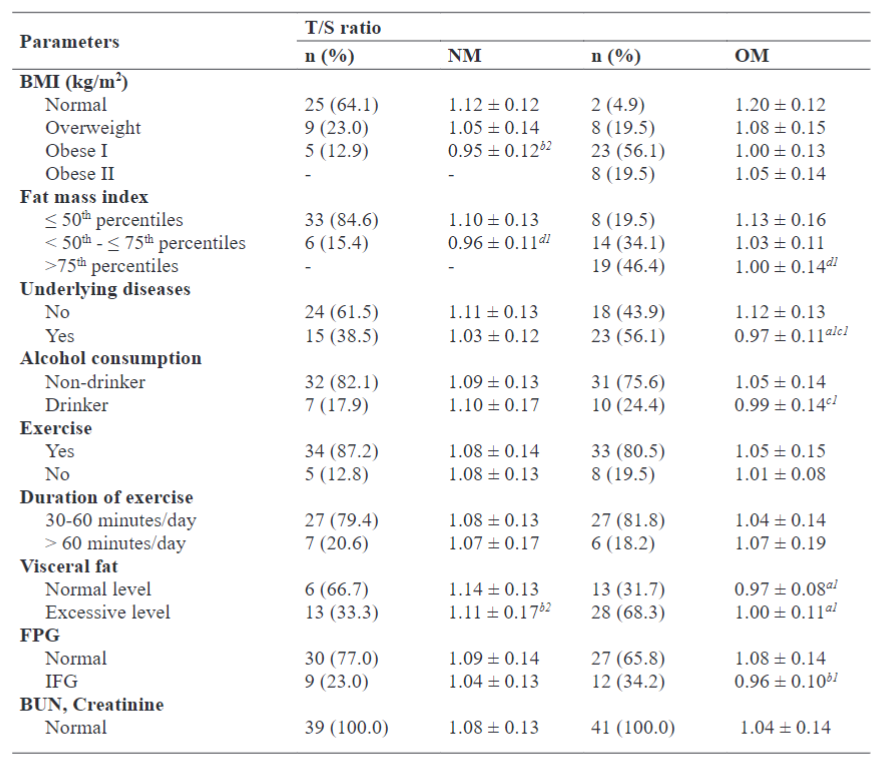
Methods: This study was a cross-sectional design including 39 normal body weight and 41 obese subjects. Nutritional status was assessed using body composition and blood biochemistry. General information and health information were obtained by using questionnaires. Telomere length was measured using the monochromatic multiplex real-time quantitative PCR (MMqPCR) and reported in T/S ratio.
Results: In both normal weight and obese groups, the mean telomere length was found to be shortest in the oldest group and tended to be longer in normal weight than obese group in other age groups (aged 21-40 years: 1.19 ± 0.12 vs 1.12 ± 0.07, aged 41-60 years: 1.08 ± 0.12 vs 1.06 ± 0.10, and aged 61-82 years: 0.96 ± 0.06 vs 0.90 ± 0.07). Mean telomere length was found to be shorter in subjects with increased visceral fat, high fasting plasma glucose, BUN, and lack of exercise.
Conclusions: The findings among Thai subjects in different age groups revealed that telomere length significantly shortens with age and was found shorter in obese subjects in the same age groups. This may deteriorate the functions of various organ systems that would lead to complications of obesity.
Downloads
References
Montpetit AJ, Alhareeri AA, Montpetit M, et al. Telomere length: a review of methods for measurement. Nurs Res. 2014;63(4):289-299.
Fouquerel E, Opresko PL. Convergence of The Nobel Fields of Telomere Biology and DNA Vol.22 No.2 (May-August 2022) 151Repair. Photochem Photobiol. 2017;93(1):229-237.
Fossel M. Use of Telomere Length as a Biomarker for Aging and Age-Related Disease. Current Translational Geriatrics and Experimental Gerontology Reports, 2012;1:121-127.
Kong CM, Lee XW, Wang X. Telomere shortening in human diseases. FEBS J. 2013;280(14):3180-3193.
World Health Organization. What is overweight and obesity? https://www.who.int/dietphysicalactivity/childhood_what/en/. Published 2017. Accessed October 15, 2019.
Epel ES. Psychological and metabolic stress: a recipe for accelerated cellular aging? Hormones (Athens). 2009;8(1):7-22.
Hertzog MA. Considerations in determining sample size for pilot studies. Res Nurs Health. 2008;31(2):180-191.
Leelahagul P, Klawisat K, Kongpun P, Udomlap J, Janthranant G, Hoiyeephoo K. Segmental bioelectrical impedance analysis in Northern Thai secondary school-age students (PCCCR). Ann Nutr Metab. 2013;63(S1):1426.
Mindray Bio-Medical Electronics Co. L. BS-400 Chemistry Analyzer. http://www.diasystem.se/uploads/9/6/6/7/9667782/
bs-400201307.pdf. Published 2013. Accessed August 27, 2018.
Gallagher D, Heymsfield SB, Heo M, Jebb SA, Murgatroyd PR, Sakamoto Y. Healthy percentage body fat ranges: an approach for
developing guidelines based on body mass index. Am J Clin Nutr. 2000;72(3):694-701.
Organization WH. The Asia-Pacific perspective: Redefining obesity and its treatment. https://apps.who.int/iris/bitstream/handle/10665/206936/0957708211_eng.pdf?sequence=1&tnqh_x0026;isAllowed=y. Published 2000. Accessed Septemper 24, 2021.
Tanita. Visceral Fat - What is Visceral Fat and why is it Important? https://tanita.eu/helpguides/understanding-your-measurements/visceral-fat/. Published 2000. Accessed October 13, 2021.
Cawthon RM. Telomere length measurement by a novel monochrome multiplex quantitative PCR method. Nucleic Acids Res. 2009;37(3):e21.
Survey NHaNE. Telomere Mean and Standard Deviation (Surplus) (TELO_B). https://www.cdc.gov/nchs/nhanes/2001-2002/TELO_B. htm. Published 2015. Accessed January 11, 2014.
Nguyen MT, Lycett K, Vryer R, et al. Telomere length: population epidemiology and concordance in Australian children aged 11-12 years and their parents. BMJ Open. 2019;9(S3):118-126.
Nonino CB, Pinhanelli VC, Noronha NY, et al. Green tea supplementation promotes leukocyte telomere length elongation in obese women. Nutr Hosp. 2018;35(3):570-575.
Charoenying T, Kruanamkam W, Yu-iam S, U-chuvadhana P, Rerksngarm T. Telomere length distribution in blood and saliva by RT-PCR in age-varying Thais: A Pilot Study. PTU Journal of Science and Technology. 2020;1(1):35-48.
Srettabunjong S, Satitsri S, Thongnoppakhun W, Tirawanchai N. The study on telomere length for age estimation in a Thai population. Am J Forensic Med Pathol. 2014;35(2):148-153.
Greider CW, Blackburn EH. A telomeric sequence in the RNA of Tetrahymena telomerase required for telomere repeat synthesis. Nature. 1989;337(6205):331-337.
Andriollo-Sanchez M, Hininger-Favier I, Meunier N, et al. Age-related oxidative stress and antioxidant parameters in middle-aged and older European subjects: the ZENITH study. Eur J Clin Nutr. 2005;59(S2):58-62.
Abdelaal M, le Roux CW, Docherty NG. Morbidity and mortality associated with obesity. Ann Transl Med. 2017;5(7):161.
Njajou OT, Cawthon RM, Blackburn EH, et al. Shorter telomeres are associated with obesity and weight gain in the elderly. Int J Obes (Lond). 2012;36(9):1176-1179.
Moreno-Navarrete JM, Ortega F, Sabater M, Ricart W, Fernandez-Real JM. Telomere length of subcutaneous adipose tissue cells is shorter in obese and formerly obese subjects. Int J Obes (Lond). 2010;34(8):1345-1348.
Poli G, Leonarduzzi G, Biasi F, Chiarpotto E. Oxidative stress and cell signalling. Curr Med Chem. 2004;11(9):1163-1182.
Hunter GR, Gower BA, Kane BL. Age Related Shift in Visceral Fat. Int J Body Compos Res. 2010;8(3):103-108.
Bays H. Central obesity as a clinical marker of adiposopathy; increased visceral adiposity as a surrogate marker for global fat dysfunction. Curr Opin Endocrinol Diabetes Obes. 2014;21(5):345-351.
Tzanetakou IP, Katsilambros NL, Benetos A, Mikhailidis DP, Perrea DN. “Is obesity linked to aging?”: adipose tissue and the role of
telomeres. Ageing Res Rev. 2012;11(2):220-229.
Hristov I, Mocanu V, Zugun-Eloae F, et al. Association of intracellular lipid accumulation in subcutaneous adipocyte precursors and plasma adipokines in bariatric surgery candidates. Lipids Health Dis. 2019;18(1):141.
Ma D, Zhu W, Hu S, Yu X, Yang Y. Association between oxidative stress and telomere length in Type 1 and Type 2 diabetic patients. J Endocrinol Invest. 2013;36(11):1032-1037.
Monickaraj F, Aravind S, Gokulakrishnan K, et al. Accelerated aging as evidenced by increased telomere shortening and mitochondrial DNA depletion in patients with type 2 diabetes. Mol Cell Biochem. 2012;365(1-2):343-350.
Percy CJ, Power D, Gobe GC. Renal ageing: changes in the cellular mechanism of energy metabolism and oxidant handling. Nephrology (Carlton). 2008;13(2):147-152.
Puterman E, Lin J, Blackburn E, O’Donovan A, Adler N, Epel E. The power of exercise: buffering the effect of chronic stress on telomere length. PLoS One. 2010;5(5):e10837.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2022 Asian Medical Journal and Alternative Medicine

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.


