Mortality Rate and Associated Factors in Critically Ill Intubated Patients with Coronavirus Disease 2019 (COVID-19) at Pranangklao Hospital
Keywords:
Anesthetics, Critical illnes, Coronavirus, COVID-19, Mortality rate, Intubation, SARS-CoV-2Abstract
Introduction: In the epidemic wave of the ongoing coronavirus disease 2019 (COVID-19) pandemic in April 2021. This study aimed to explore the 30-day mortality rate and its associated factors and anesthetic practice in critically ill COVID-19 patients who received intubation.
Methods: This retrospective cohort study was collected data from medical records in critically ill COVID-19 patients who received intubation and admitted to Pranangklao Hospital (PNKH) from April 1 to June 30, 2021.
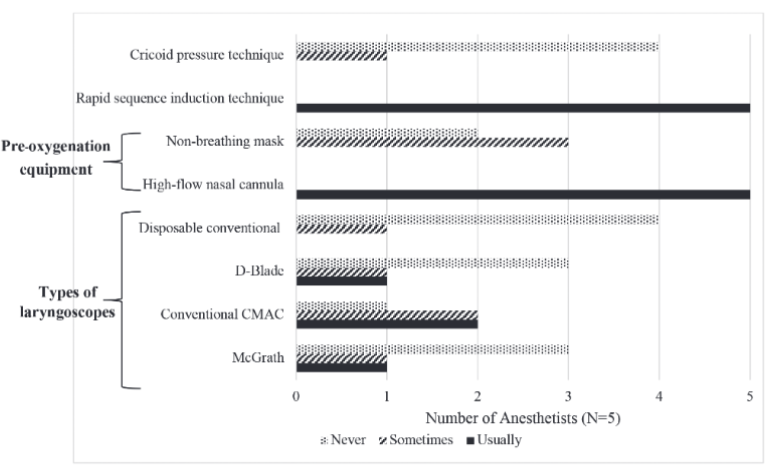
Results: A total of 73 patients were admitted and intubated with the median age was 65 years (IQR = 18), 43 (58.9%) were male, 37 (50.7%) were body mass index (BMI) ≥ 30 kg/m2, and 60 (82.2%) had underlying diseases. The most common underlying diseases were hypertension (63.00%) and diabetes (47.90%). The 30-day mortality rate was 79.50%. Compared between the survivors (n = 15) and non-survivors (n = 58), the mortality significantly increased with age (P = .002), more underlying diseases (P = .007), having cough (RRadj 31.90, 95% CI = 1.67-610.65, P = .021), and more complications (RRadj 2.58, 95% CI = 1.02-6.51, P = .045). The anesthetics were used as follows: midazolam (80.95%), thiopental (40.48%), propofol (26.19%), and ketamine (23.81%). The muscle relaxants used in intubation included succinylcholine (90.48%) and rocuronium (9.52%).
Conclusions: Critically ill intubated COVID-19 patients showed a very high mortality rate that significantly increased with age, underlying diseases, and complications. Intubation treatment in vulnerable populations should be done cautiously to avoid adverse events.
Downloads
References
Lu H, Stratton CW, Tang YW. Outbreak of pneumonia of unknown etiology in Wuhan, China: The mystery and the miracle. Journal of medical virology. 2020;92(4):401-402.
Hui DS, E IA, Madani TA, et al. The continuing 2019-nCoV epidemic threat of novel coronaviruses to global health-The latest 2019 novel coronavirus outbreak in Wuhan, China. International journal of infectious diseases : IJID : official publication of the International Society for Infectious Diseases. 2020;91:264-266.
World Health Organization. Novel Coronavirus-Thailand (ex-China). World Health Organization. https://www.who.int/emergencies/disease-outbreak-news/item/2020-DON234. Updated January 14, 2020. Accessed July 25, 2021.
World Health Organization. Novel Coronavirus 2019 (nCoV) Situation Report -1. World Health Organization. https://www.who.int/docs/default-source/coronaviruse/situationreports/20200121-sitrep-1-2019-ncov.pdf. Updated January 20, 2020. Accessed July 25, 2021.
Emergency Situation Center DoDC. The Coronavirus Disease 2019 Situation, Thailand situation. Emergency Situation Center DoDC. https://ddc.moph.go.th/viralpneumonia/eng/file/situation/situation-no357-311263.pdf. Updated December 31, 2020. Accessed July 25, 2021.
Daniel WW. A foundation for analysis in the health sciences. Biostatistics Toronto, John Wiley & Sons. 1991;209-215.
Ngamjarus C, Chongsuvivatwong V. N4Studies: Sample size and power calculations for iOS. The Royal Golden Jubilee Ph D Program-The Thailand Research Fund & Prince of Songkla University. 2014.
Tu Y, Yang P, Zhou Y, et al. Risk factors for mortality of critically ill patients with COVID-19 receiving invasive ventilation. International journal of medical sciences. 2021;18(5):1198-1206.
Petrilli CM, Jones SA, Yang J, et al. Factors associated with hospital admission and critical illness among 5279 people with coronavirus
disease 2019 in New York City: prospective cohort study. BMJ (Clinical research ed). 2020;369:1966.
Halvatsiotis P, Kotanidou A, Tzannis K, et al. Demographic and clinical features of critically ill patients with COVID-19 in Greece: The burden of diabetes and obesity. Diabetes research and clinical practice. 2020;166:108331.
Du RH, Liang LR, Yang CQ, et al. Predictors of mortality for patients with COVID-19 pneumonia caused by SARS-CoV-2: a prospective
cohort study. The European respiratory journal. 2020;55(5):2000524.
The Royal College of Anesthesiologist of Thailand. Current practice guideline for anesthesia management in COVID-19 case. The Royal College of Anesthesiologist of Thailand. https://www.rcat.org/cpg?lang=en. Published April 24, 2020. Accessed September 26, 2021.
Cervantes J, Sureen A, Galura G, et al. Factors associated with COVID-19 severity and mortality among Hispanic patients living on the USA–Mexico border. Journal of Investigative Medicine. 2021;69(4):819.
Dessie ZG, Zewotir T. Mortality-related risk factors of COVID-19: a systematic review and meta-analysis of 42 studies and 423, 117 patients. BMC Infectious Diseases. 2021;21(1):855.
Grasselli G, Zangrillo A, Zanella A, et al. Baseline Characteristics and Outcomes of 1591 Patients Infected With SARS-CoV-2 Admitted
to ICUs of the Lombardy Region, Italy. Jama. 2020;323(16):1574-1581.
Watson RA, Pride NB, Thomas EL, et al. Reduction of total lung capacity in obese men: comparison of total intrathoracic and
gas volumes. Journal of applied physiology (Bethesda, Md : 1985). 2010;108(6):1605-1612.
Dixon AE, Peters U. The effect of obesity on lung function. Expert review of respiratory medicine. 2018;12(9):755-767.
Cai Q, Chen F, Wang T, et al. Obesity and COVID-19 Severity in a Designated Hospital in Shenzhen, China. Diabetes care. 2020;43(7):1392-1398.
Simonnet A, Chetboun M, Poissy J, et al. High Prevalence of Obesity in Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2) Requiring Invasive Mechanical Ventilation. Obesity (Silver Spring, Md). 2020;28(7):1195-1199.
Nakeshbandi M, Maini R, Daniel P, et al. The impact of obesity on COVID-19 complications: a retrospective cohort study. International journal of obesity (2005). 2020;44(9): 1832-1837.
Cai Z, Yang Y, Zhang J. Obesity is associated with severe disease and mortality in patients with coronavirus disease 2019 (COVID-19):a meta-analysis. BMC Public Health. 2021;21(1):1505.
Centers for Disease Control and Prevention. Defining adult overweight and obesity. Division of Nutrition, Physical Activity, and Obesity, National Center for Chronic Disease Prevention and Health Promotion. https://www.cdc.gov/obesity/adult/defining.html.
Updated June 7, 2021. Accessed 20 October, 2021.
World Obesity Federation. Obesity. World Health Organization. https://www.who.int/news-room/fact-sheets/detail/obesity-andoverweight. Accessed October 20, 2021.
Kim EJ, Ha KH, Kim DJ, Choi YH. Diabetes and the Risk of Infection: A National Cohort Study. Diabetes & metabolism journal. 2019;43(6):804-814. Vol.22 No.2 (May-August 2022) 137
Hur K, Price CPE, Gray EL, et al. Factors Associated With Intubation and Prolonged Intubation in Hospitalized Patients With COVID-19. Otolaryngology--head and neck surgery : official journal of American Academy of Otolaryngology-Head and Neck Surgery. 2020;163(1):170-178.
Kumar A, Arora A, Sharma P, et al. Is diabetes mellitus associated with mortality and severity of COVID-19? A meta-analysis. Diabetes & metabolic syndrome. 2020;14(4):535-545.
Guo W, Li M, Dong Y, et al. Diabetes is a risk factor for the progression and prognosis of COVID-19. Diabetes/metabolism research and reviews. 2020;3319.
Abdi A, Jalilian M, Sarbarzeh PA, Vlaisavljevic Z. Diabetes and COVID-19: A systematic review on the current evidences. Diabetes
research and clinical practice. 2020;166:108347.
Loushin MK. The Effects of Anesthetic Agents on Cardiac Function. In: Iaizzo PA, ed. Handbook of Cardiac Anatomy, Physiology, and Devices. Humana Press;2005:171-180.
Ghia S, Lazar M, Epstein J, Bhatt HV. “Anesthesia Stat” to Intubate a Coronavirus Disease 2019 (COVID-19) Patient: Implications for the Anesthesiologist. Journal of cardiothoracic and vascular anesthesia. 2020;34(10):2566-2570.
Weinbroum AA. Perspectives of Ketamine Use in COVID-19 Patients. Journal of Korean medical science. 2021;36(4):28.
Ortoleva J. Consider Adjunctive Ketamine in Mechanically Ventilated Coronavirus Disease-2019 Patients. Journal of cardiothoracic and vascular anesthesia. 2020;34(10):2580.
Hirota K, Lambert DG. Anaesthesia-related drugs and SARS-CoV-2 infection. British journal of anaesthesia. 2021;127(1):32-34.
Suri A, Sindwani G. Ketamine use in the COVID-19 era: be cautious! Korean journal of anesthesiology. 2020;73(6):568-569.
Brull SJ, Kopman AF. Clarifications on Technologies to Optimize Care of Severe COVID-19 Patients. Anesthesia and analgesia. 2020;131(4):192-193.
Ministry of Public Health. COVID-19 Vaccination Report. Ministry of Public Health. https://ddc.moph.go.th/vaccine-covid19/diaryPresentMonth/07/10/2021. Updated July 1, 2021. Accessed September 23, 2021.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2022 Asian Medical Journal and Alternative Medicine

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.


